
Impact of sex differences in co‐morbidities and medication adherence on outcome in 25,776 heart failure patients using a health insurance claims database
Randomised controlled trials (RCT) in chronic heart failure (CHF) usually have a select patient population, where women and those with multi-morbidity are often underrepresented. Therefore, the use of big data is becoming increasingly more popular in epidemiological research to better cover the heterogeneity. Health insurance claims (HIC) databases capture the unselected Dutch patient population, which makes them suitable for studying the sex-specific effects of comorbidities and medication adherence on prognosis.
The authors of this research analysed the Achmea HIC database including 14,517 men and 11,259 (45%) women with CHF, relating patients characteristics with the primary endpoint (PE) of all-cause mortality or HF admission. They show that in this large HIC database, capturing a representative sample of the Dutch population, men with CHF had a 25% increased risk of the PE than women. Furthermore, a broad range of comorbidities was associated with the PE. The impact of comorbidities was sex-dependent, with a stronger association in women than in men, particularly for renal insufficiency, COPD/Asthma, and diabetes, whereas adherence to heart failure medication was not sex-dependent.
The results underscore the merit of HIC databases in CHF as an addition to RCT data and demonstrate that additional research into sex differences in heart failure is warranted. Treatment should move towards a more patient-tailored approach and the use and value of HIC database should be further evaluated.
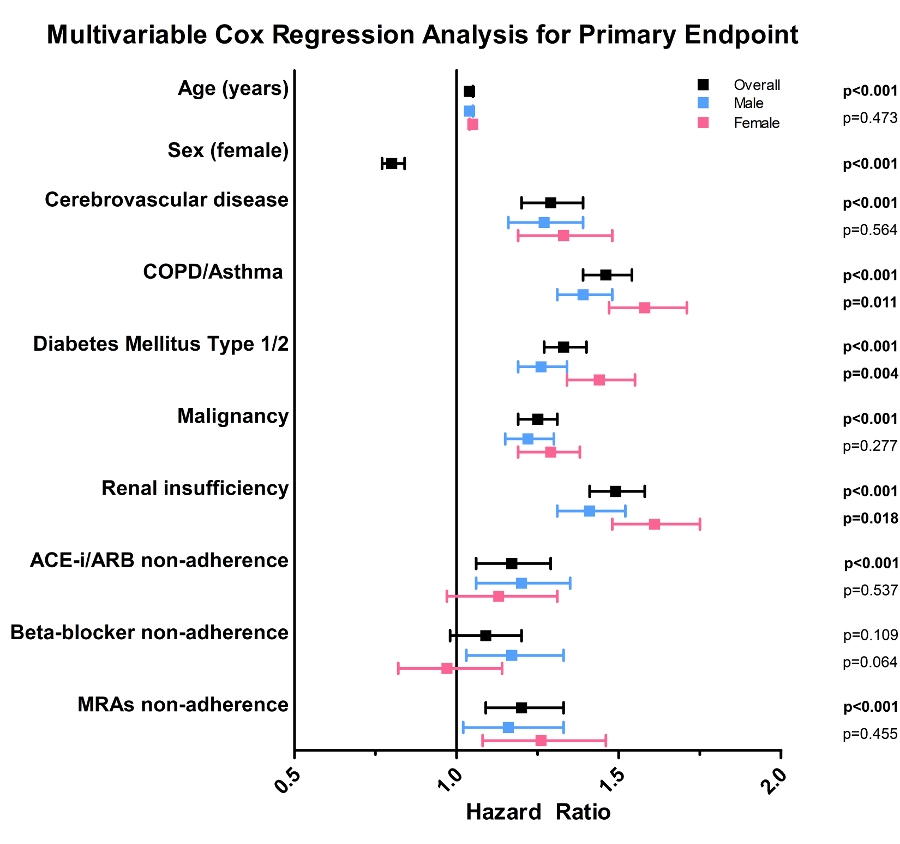
Coefficient plot of hazard ratio’s with corresponding 95% confidence intervals. Overall results are based on a single multivariable cox regression analysis with 27 variables (including sex) in relation to the primary endpoint. Potential effect modification by sex was assessed by including an interaction term between sex and the variable of interest in separate multivariable cox regression analyses. ACE-i, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; COPD, chronic obstructive pulmonary disease; MRA, mineralocorticoid receptor antagonist. Significant P-values are in bold.
The paper ‘Impact of sex differences in co‐morbidities and medication adherence on outcome in 25 776 heart failure patients‘, conducted by researchers from Erasmus University Medical Center (Erasmus MC) and Achmea, has been published in ESC Heart Failure. Access the paper here.

